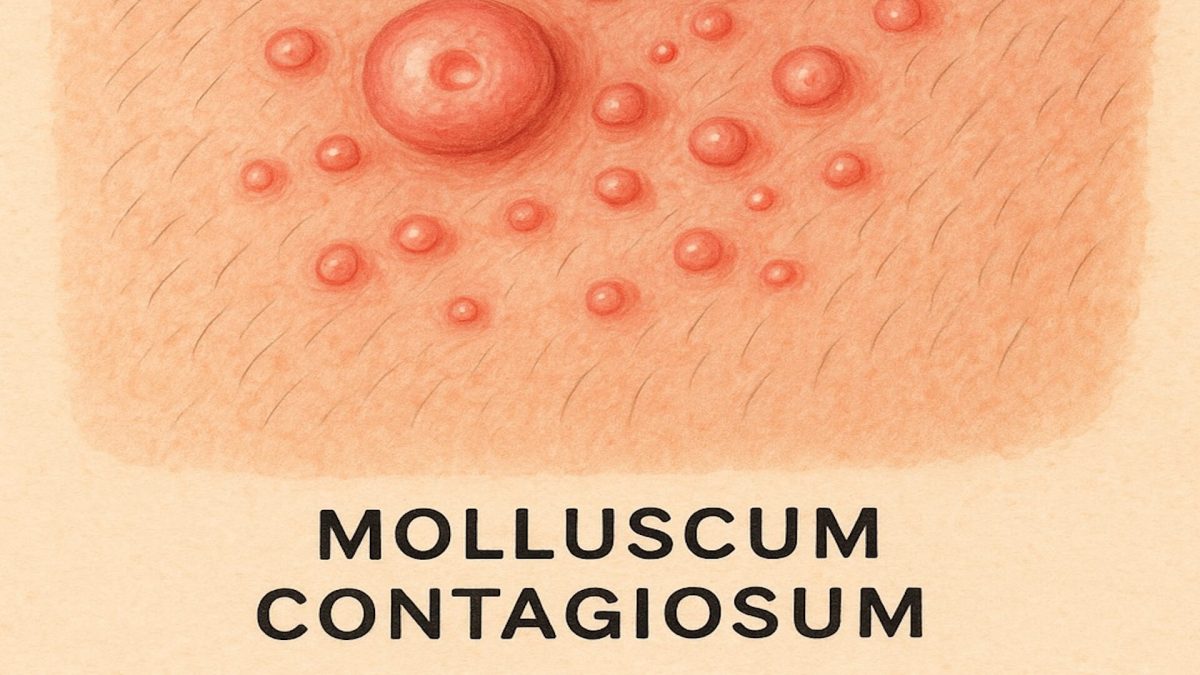
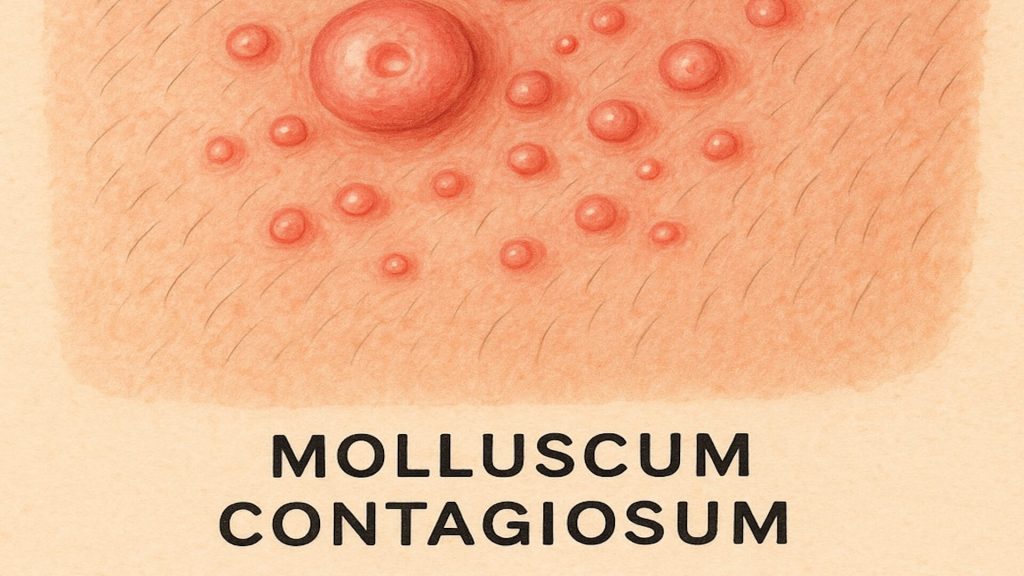
Molluscum contagiosum is a common viral skin infection that presents as small, dome-shaped papules. It can affect children, adults, and individuals with specific risk factors. Though often harmless, its appearance may cause discomfort or cosmetic concern.
This article explains how molluscum contagiosum develops, its symptoms, transmission routes, and recognised treatment options for safe and effective management.
What Is Molluscum Contagiosum
Molluscum contagiosum is caused by the molluscum contagiosum virus, a member of the Poxviridae family. It produces smooth, raised, flesh-coloured lesions with a central dimple known as mollusca.
These lesions typically measure between 2 and 5 mm in diameter and are most common in children aged 1 to 10, though adults can also be affected. The infection usually clears within 6 to 12 months but may persist longer in individuals with weakened immune systems such as those living with HIV [1,2,3].
Molluscum contagiosum spreads easily in communal settings like swimming pools and playgrounds, and through close skin contact during activities or intimacy [2,4,6].
How Molluscum Contagiosum Spreads
Molluscum contagiosum spreads through direct skin contact with infected lesions or by touching contaminated objects such as towels, clothing, or toys [1]. Scratching can also spread the virus to other areas of the body, known as autoinoculation [3].
Among adults, sexual contact is a common route of transmission, leading to lesions in the genital or lower abdominal area [4]. Preventive care such as covering lesions, avoiding shared items, and maintaining hygiene significantly reduces transmission risk.
Recognising Molluscum Contagiosum Symptoms
Typical Lesion Appearance
The hallmark sign is a cluster of small, raised, flesh-coloured papules with a smooth surface and central indentation [1]. These are typically painless but may become itchy or inflamed if irritated.

Secondary Skin Changes
In some cases, eczema or mild redness develops around lesions, signalling the body’s immune response [3]. Avoiding scratching is important to prevent bacterial infection or scarring during healing.
Commonly Affected Areas
| Age Group | Typical Locations |
|---|---|
| Children | Face, neck, arms, and hands |
| Adults | Genital area, lower abdomen, inner thighs |
Table 1: Common lesion sites and age-related patterns
Diagnosing Molluscum Contagiosum
Healthcare professionals diagnose molluscum contagiosum primarily through clinical examination [1]. The condition’s distinct appearance usually eliminates the need for further tests.
If uncertainty arises, a biopsy may confirm the diagnosis by identifying Henderson-Patterson bodies, which are microscopic inclusions specific to this virus [3]. Accurate diagnosis ensures appropriate care and reassurance.
Treatment For Molluscum Contagiosum
Although the condition often clears naturally, treatment may be recommended to shorten duration, ease symptoms, or prevent spread. A healthcare professional can advise on suitable options.
| Treatment Method | Description | Benefits | Considerations |
|---|---|---|---|
| Topical Treatments | Application of solutions such as potassium hydroxide or salicylic acid [3] | Non-invasive and can accelerate clearance | May cause redness or irritation |
| Physical Removal | Cryotherapy or curettage to remove lesions [1] | Immediate lesion reduction | Temporary discomfort or mild scarring possible |
| Oral Medications | Immunomodulatory therapy in select severe cases [5,6] | May reduce lesion count in immunocompromised patients | Used only under supervision |
Table 2: Evidence-based treatment options for molluscum contagiosum
Preventing Molluscum Contagiosum
Good hygiene and protective habits help prevent transmission and reinfection.
| Preventive Measure | Description |
|---|---|
| Avoid Sharing Personal Items | Do not share towels, clothing, or personal care objects |
| Cover Lesions | Use waterproof dressings or clothing, especially during swimming [2] |
| Practice Safe Contact | Maintain hygiene during intimacy or sports [4] |
| Wash Hands Regularly | Reduces autoinoculation and spread to others [1] |
Table 3: Preventive measures to limit transmission and reinfection
When To Seek Medical Advice
Molluscum contagiosum is self-limiting, but medical review is advised if:
- Lesions appear in the genital area [4]
- You have a weakened immune system [3]
- Lesions become painful, inflamed, or infected [1]
- The condition persists beyond 18 months [2]
Professional assessment ensures correct diagnosis and supports safe management.
Monderma’s Role In Skin Health
For individuals managing conditions such as acne, rosacea, or pigmentation, Monderma’s personalised skincare offers prescription-strength treatments designed by UK-registered prescribers. Each formulation is developed following an online clinical consultation to ensure suitability, safety, and results.
Molluscum contagiosum is viral and should be managed through medical care. Monderma’s treatments are designed to complement overall skin health but are not used to treat viral infections.
Conclusion
Molluscum contagiosum is a mild viral skin infection that often resolves naturally but may require treatment to prevent spread or discomfort. Understanding its symptoms, causes, and treatment options empowers individuals to manage their skin confidently and safely.
Practising good hygiene and seeking professional advice support faster recovery and protect others from infection. Explore Monderma’s free consultation to receive expert guidance on maintaining healthy, resilient skin.
Content is for informational purposes only. Monderma treatments are prescribed following consultation. Results and timeframes can vary. Use as directed by your prescriber.
Bibliography
- NHS. Molluscum contagiosum. NHS Website. Published February 18, 2020.
- CDC. Molluscum Contagiosum. CDC Website.
- CDC. Clinical Overview of Molluscum Contagiosum. Published April 15, 2025.
- CDC. Preventing Molluscum Contagiosum in Schools, Daycares, and Pools. Accessed July 2025.
- NHS Lothian. Molluscum Contagiosum – RefHelp.
- Meza-Romero R., Navarrete-Dechent C., Downey C. Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol. 2019;12:373–381.