- Cystic acne causes deep, painful lesions that can scar
- Hormonal fluctuations & genetics drive most cystic acne cases
- Topical retinoids & oral antibiotics reduce inflammation effectively
- Isotretinoin treats severe cystic acne under medical supervision
- Monderma offers personalised care to manage cystic acne safely
Cystic acne is one of the most severe forms of acne vulgaris, developing deep beneath the skin and often leading to pain, swelling, and long-term scarring if untreated.
In this article, we discuss the causes, healing stages, and effective management strategies that can help reduce flare-ups and support long-term skin health.

What Is Cystic Acne?
Cystic acne involves large, pus-filled cysts that form deep within the skin, unlike surface-level blackheads or whiteheads. These lesions can persist for weeks or even months and often leave scars due to their depth [1].
Cystic acne affects around 9% of the global population, primarily adolescents aged 12 to 24 years [2]. It’s less common than mild acne but significantly more severe, often requiring medical attention and prescription treatments.
Causes Of Cystic Acne
Cystic acne arises when pores become blocked with excess oil, bacteria (Cutibacterium acnes), and dead skin cells. This blockage leads to inflammation, swelling, and deep cyst formation [3].
| Cause | Details |
|---|---|
| Hormonal Changes | Hormonal fluctuations during puberty, menstrual cycles, or PCOS increase androgens, raising sebum levels [4]. |
| Genetics | A family history of cystic acne raises risk due to inherited oil production and inflammatory tendencies [3]. |
| Diet | High-glycaemic foods and dairy products may worsen acne, though evidence remains mixed [5]. |
| Stress | Elevated cortisol can stimulate oil glands and aggravate inflammation [3]. |
Table 1: Common causes and contributing factors of cystic acne
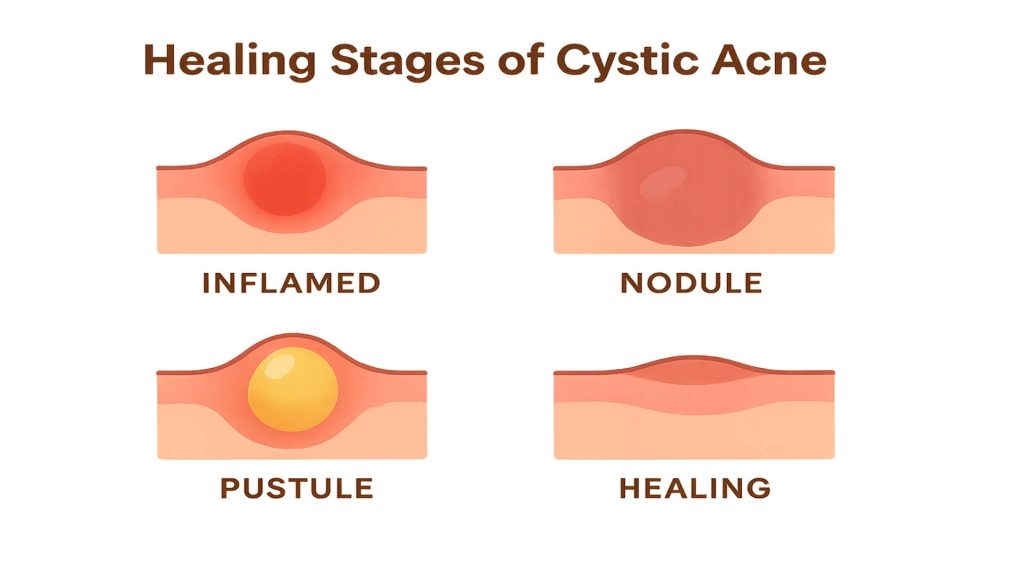
Healing Stages Of Cystic Acne
Recognising the stages of cystic acne supports better treatment timing and scar prevention.
| Stage | Characteristics | Management Tips |
|---|---|---|
| Early Stage | A red, tender lump begins forming beneath the skin. | Avoid squeezing; use gentle cleansers and apply topical antibacterial agents [1,3]. |
| Active Stage | The cyst enlarges, becoming inflamed and painful. | Topical antibiotics or retinoids help reduce inflammation; consult a dermatologist for severe cases [4]. |
| Healing Stage | The cyst shrinks, pain reduces, and pigmentation may appear. | Use non-comedogenic moisturisers and SPF to reduce hyperpigmentation risk [5]. |
Table 2: Stages of cystic acne and recommended management approaches
Effective Cystic Acne Treatments
Cystic acne often requires a combination of topical and oral treatments to control inflammation, reduce bacteria, and balance oil production.
Topical Treatments
Benzoyl Peroxide
Reduces bacteria and inflammation. Studies show a 63% lesion reduction after 12 weeks of tretinoin gel use; combining benzoyl peroxide with retinoids enhances results [6].
Salicylic Acid
Unclogs pores and exfoliates surface layers, improving mild to moderate acne [4]. Best used alongside other treatments for deeper cysts.
Topical Retinoids (Adapalene, Tretinoin)
Promote cell turnover and prevent pore blockage. Adapalene 0.1% with benzoyl peroxide 2.5% is a recommended first-line therapy for mild to moderate acne [6].
Azelaic Acid
Gentle and safe for sensitive or pregnant patients, offering antimicrobial and anti-inflammatory benefits. It also helps fade post-inflammatory hyperpigmentation [4,5].
Oral Medications
Oral Antibiotics (e.g., Doxycycline)
Reduce bacteria and inflammation. Typically prescribed for up to 3 months alongside topical treatments to avoid antibiotic resistance [5].
Combined Oral Contraceptives
Help regulate hormone levels and reduce sebum production in women with hormonal acne [2].
Isotretinoin
A potent retinoid that drastically reduces oil production and acne lesions. Reserved for severe or resistant cystic acne due to side effects and monitoring needs [3].
Lifestyle & Home Remedies
Dietary Adjustments
Reducing dairy and high-glycaemic foods may improve acne in some individuals, though responses vary [5].
Stress Management
Meditation, exercise, and mindfulness may indirectly help regulate oil production by reducing cortisol [3].
Skincare Routine
Use gentle, non-comedogenic cleansers and moisturisers. Avoid harsh scrubs or alcohol-based toners that can worsen irritation [5].
Treating Acne Scars
Cystic acne can cause scarring, especially if cysts are picked or squeezed. Dermatological procedures can improve texture and tone.
| Treatment | Mechanism | Benefits | Considerations |
|---|---|---|---|
| Chemical Peels | Remove surface layers with acids like salicylic or glycolic [3]. | Improves texture and hyperpigmentation. | May cause irritation; multiple sessions needed. |
| Laser Therapy | Stimulates collagen regeneration. | Effective for deep scars. | Higher cost; requires specialist. |
| Microneedling | Promotes collagen to smooth skin texture [3]. | Minimally invasive, effective for rolling scars. | Several sessions required. |
| Home Treatments | Silicone sheets and vitamin C serums may fade scars [5]. | Accessible and non-invasive. | Gradual results. |
Table 3: Treatment options for improving acne scars
Monderma’s Personalised Skincare Solutions
Monderma provides prescription-strength skincare tailored to acne, pigmentation, and rosacea. Custom formulations may include:
- Adapalene or Tretinoin for cell turnover.
- Azelaic Acid or Clindamycin to reduce bacteria and inflammation.
- Niacinamide to strengthen the skin barrier and soothe irritation.
Each prescription is reviewed by GPhC-registered prescribers to ensure safety and effectiveness. Through a free consultation, Monderma designs bespoke regimens that align with dermatological guidelines.
When To See A Dermatologist
Seek professional advice if:
- Acne is painful, cystic, or leaves scarring.
- Over-the-counter treatments fail after several months.
- Breakouts cause emotional distress or self-esteem issues.
NICE recommends referral for nodulocystic acne unresponsive to two 4–6-month treatment courses or causing severe distress [5]. Dermatologists can prescribe isotretinoin or advanced therapies when appropriate.
Conclusion
Cystic acne requires a comprehensive approach that combines medical treatments, skincare, and lifestyle management. Understanding its causes and healing stages helps control flare-ups, reduce scarring, and improve skin health.
For evidence-based, tailored skincare, Monderma offers free consultations to create personalised regimens that target cystic acne safely and effectively. Share this article to help others manage acne confidently and find solutions backed by clinical expertise.
Content is for informational purposes only. Monderma treatments are prescribed following consultation. Results and timeframes can vary. Use as directed by your prescriber.
Bibliography
- StatPearls. Acne Vulgaris. NCBI Bookshelf. Updated 2023.
- Eichenfield DZ, Sprague J, Eichenfield LF. Management of Acne Vulgaris: A Review. JAMA. 2021;326(20):2055–2067.
- Zaenglein AL, et al. Guidelines of Care for the Management of Acne Vulgaris. J Am Acad Dermatol. 2016;74(5):945–973.
- Reynolds RV, et al. Guidelines of Care for the Management of Acne Vulgaris. J Am Acad Dermatol. 2024;90(5):1006.e1–1006.e30.
- National Institute for Health and Care Excellence (NICE). Acne Vulgaris: Management. NG198. 2021.
- Chandrashekhar BS, et al. Tretinoin Nanogel 0.025% Versus Conventional Gel 0.025% in Acne Treatment. Indian J Dermatol. 2015;60(5):520.
Find your perfect skincare formula
Takes less than 2 minutes – see what your skin needs
Get Custom Formula